COVID-19 Mortality Rate: Separating Fact from Sensationalism
Updated August 2023
With the advantage of hindsight, let’s revisit this story. When this article was initially published, it coincided with the peak of panic in September 2020. While we’ve added new insights, the fundamental lesson remains clear: panicking and blindly following the crowd has historically proven to be unwise. They were wrong then, are wrong now, and will likely continue to be wrong in the future.
Hysteria has gripped everyone, especially in the US and it’s feeding on itself. When you add in the elect officials’ stupidity and ineptitude, what should have been a mild situation turned into a nightmare-type scenario. We are supposedly the most advanced nation on earth, but after the current debacle, one would be hard-pressed to call the US advanced, at least in the medical arena. Had the US taken the same stance as South Korea, the markets would have fared much better, and people would have panicked less because they would have felt that the situation was under control. The testing delay turned a nervous crowd into a hysterical mob.
Let’s address the prominent headlines the press is trying to promote, claiming that coronavirus cases have surged in New York. It’s essential to recognize that such a spike is expected when you increase testing. This narrative is misleading, and the media should prioritize factual reporting.
While the coronavirus mortality rate may be on the rise, it still pales in comparison to the devastating impact of diseases like cancer and the harmful effects of smoking, which claim more lives than COVID-19. It’s crucial to consider these facts when evaluating the current situation.
Misleading Media Spin: Understanding Coronavirus Mortality Rates
If we calculate the death rate, it currently stands at 1.28%. However, rather than emphasizing this fact, there is an inclination to portray the recent spike in coronavirus cases as a shocking development. It’s important to acknowledge that increased testing contributes to this spike, as it involves a larger pool of people, including those with milder or asymptomatic cases.
Unfortunately, the media tends to highlight the negative aspects and may exaggerate a situation that remains manageable. Nowhere is this more evident than in Italy, which we will discuss shortly. Despite the surge in the number of cases, the coronavirus mortality rate remains relatively stable across all groups.
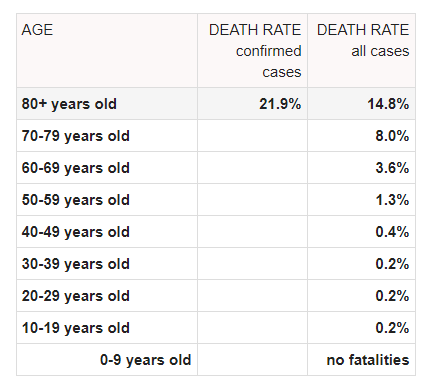
The table illustrates that those with pre-existing conditions are the ones most at risk.
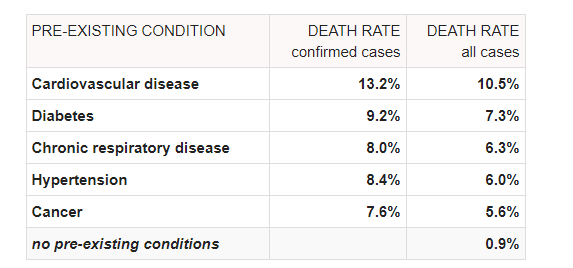
Coronavirus mortality rate across all age groups
What truly stands out is that the Coronavirus mortality rate drops to 0.9% across all age groups when individuals have no pre-existing conditions. This crucial statistic deserves widespread attention instead of being obscured. Thus, it’s evident that age alone is not the sole determining factor; rather, it’s the combination of age and pre-existing conditions that plays a predominant role.
Regrettably, we have witnessed the United States reacting in a disconcerting manner. Instead of providing stability during this challenging time, the myriad of conflicting orders and directives from different governors and agencies has fostered anxiety rather than hope. The recent market pullbacks cannot be attributed to underlying economic conditions but rather to the pervasive feeling that there is a lack of coordinated action.
The need for mass testing centers, akin to those in New York, is imperative to regain control. Disinformation has become rampant, and I personally embarked on a journey to Asia without prior announcement to investigate and offer Tactical Investors a clearer perspective. My travels took me to Vietnam, Malaysia, Cambodia, Singapore, and Indonesia, and I can assert with confidence that Asia is handling the psychological aspects of this situation far more effectively than the West. Panic-buying and emptying shelves are not prevalent; the most sought-after items are face masks. The contrast in the psychological approach between Asia and the West is striking.
The Impact of Coronavirus Mortality Rate on Public Response and Stress Management
Subtitle: “Coronavirus Mortality Rate: Shaping Public Response and Stress Management”
For instance, Jakarta is on the brink of declaring a state of emergency, yet there is no widespread panic. In a similar vein, Malaysia is taking measures to close its borders. Surprisingly, the most significant reaction has been Malaysians working in Singapore returning home to gather additional supplies and then returning to Singapore for an extended stay. Many Malaysians commute daily from Singapore to Malaysia, and the prospect of border closures has prompted them to ensure they have enough essentials for their prolonged stay in Singapore.
If Western leaders, particularly in the United States, could adopt a similar approach to instill calm among the populace, the response would likely differ significantly. Fear intensifies stress, and prolonged stress weakens the immune system. The comprehensive data presented below clearly underscores the potential lethality of stress, particularly among older individuals who often have underlying health conditions. Additional anxiety places an added burden on already weakened immune systems.
During acute stress episodes lasting only minutes, specific types of cells are mobilized into the bloodstream, potentially preparing the body for injury or infection during the “fight or flight” response [1]. Acute stress also elevates blood levels of pro-inflammatory cytokines [2]. On the other hand, chronic stress, which can persist for days to years, like acute stress, is linked to higher levels of pro-inflammatory cytokines but may have distinct health consequences [3]. While short-term inflammation is essential for eliminating pathogens and initiating healing, chronic, systemic inflammation signifies immune system dysregulation and heightens the risk of chronic diseases such as atherosclerosis and frailty [4]. Another consequence of chronic stress is the activation of latent viruses. The reactivation of latent viruses can indicate a loss of immunological control over the virus, and frequent reactivation can lead to wear and tear on the immune system [5]. ncbi.nlm.nih.gov
Moreover, stress reduces the body’s lymphocyte count, which comprises white blood cells crucial for combating infections. When your lymphocyte level drops, your vulnerability to viruses, including common colds and cold sores, increases.
The Impact of Chronic Stress on Immune Health
Chronic stress takes a toll on our well-being, leading to depression and anxiety, which, in turn, elevate inflammation levels. Over the long term, this persistent and heightened inflammation signifies an overworked and fatigued immune system that struggles to provide adequate protection. [Source: Cleveland Clinic](https://cle.clinic/3bct0xx)
Continual stress renders us vulnerable to illnesses and diseases because it prompts the brain to signal the endocrine system, which then releases a cascade of hormones. While these hormones prepare us for emergency situations, they also severely compromise our immunity. Some experts assert that stress may be responsible for as much as 90% of all illnesses and diseases, including cancer and heart disease. It accomplishes this by triggering chemical reactions and inundating the body with cortisol, which, among other effects, reduces inflammation, diminishes white blood cells and NK cells (specialized cancer-killing cells), enhances tumour development and growth, and elevates the risk of infection and tissue damage. https://bit.ly/2U9yNOw
It has become well-accepted in recent decades that psychological stress can adversely affect many aspects of immune function (Glaser and Kiecolt-Glaser, 2005). However, the full health impact of stress may not be fully revealed until the effects of ageing are more widely appreciated. Chronic stress may speed the rate of normal age-related immune dysregulation (Kiecolt-Glaser and Glaser, 2001; Sapolsky et al., 1986). Moreover, age-related disease and impairment may augment the effects of stress or result in more significant clinical impairment for older individuals (Hawkley and Cacioppo, 2004; Kiecolt-Glaser and Glaser, 2001). https://bit.ly/2QyZqdw
The Intersection of Ageing, Immune Function, and Chronic Stress
Ageing is inherently linked to a natural decline in immune functionality, a phenomenon known as immunosenescence. This decline manifests in various aspects of both innate and adaptive immunity. For instance, older individuals exhibit a diminished natural killer cell (NK) response to stimulatory cytokines compared to their younger counterparts [1]. Ageing also leads to impaired activation and proliferation of T- and B-lymphocytes [2]. Additionally, B-lymphocytes in elderly individuals produce fewer antibodies than those in younger individuals [3]. Furthermore, ageing is associated with an increased production of specific inflammatory mediators [4]. These immunological changes render older individuals more susceptible to a range of age-related diseases.
However, when immunosenescence is compounded by the accumulation of chronic illnesses, recurrent infections, or other external factors, older individuals face an even greater risk [5]. Chronic stress may be one of the factors that render elderly individuals more vulnerable to age-related diseases [6,7]. https://bit.ly/33y4pRg
Stress and Its Pervasive Impact on Immune Health: Implications for the Elderly
In the early 1980s, psychologist Janice Kiecolt-Glaser, PhD, and immunologist Ronald Glaser, PhD, both from the Ohio State University College of Medicine, were captivated by animal studies suggesting a link between stress and infection. Between 1982 and 1992, these pioneering researchers conducted a comprehensive study involving medical students. Among their findings, they discovered that the students’ immune responses deteriorated each year during the stressful three-day exam period. Test-takers exhibited reduced numbers of natural killer cells, which combat tumors and viral infections. Furthermore, they nearly ceased producing gamma interferon, an immunity-enhancing substance, and their infection-fighting T-cells displayed weak responses to stimulation in test tubes.
These groundbreaking findings spurred a wave of research in this field. By 2004, Suzanne Segerstrom, PhD, from the University of Kentucky, and Gregory Miller, PhD, from the University of British Columbia, had reviewed nearly 300 studies on stress and health. Their meta-analysis unveiled compelling patterns. Laboratory studies that induced stress for short durations showed a surge in one type of “first responder” activity but also revealed signs of overall immune weakening. However, when stress persisted for extended periods, ranging from days to months or even years, as commonly occurs in real-life situations, all aspects of the immune system experienced a decline. Thus, chronic or long-term stress, due to excessive wear and tear, can have detrimental effects on the immune system.
Now, if stress can suppress the immune systems of healthy individuals, its impact on the elderly, who tend to experience more anxiety and often have underlying conditions (especially if they adhere to a modern-day diet), is likely even more pronounced. In the event they encounter a virus or bacteria with heightened strength, these effects could potentially become life-threatening.
Stress and the Vulnerability of Older Immune Systems
The meta-analysis also illuminated the fact that older individuals or those who are already in ill health are more susceptible to stress-induced changes in their immune systems. A 2002 study conducted by Lyanne McGuire, PhD, from the John Hopkins School of Medicine in collaboration with Kiecolt-Glaser and Glaser underscored this point. The study focused on individuals in their early 70s who were providing care for someone with Alzheimer’s disease. The research found that even chronic, sub-clinical mild depression could suppress the immune system in older individuals. Specifically, participants with chronic mild depression exhibited weaker lymphocyte-T cell responses to two mitogens, which stimulate the body’s reactions to viruses and bacteria. This immune response remained subdued even 18 months later, and immunity continued to decline with age. In accordance with the 2004 meta-analysis, it became apparent that the critical factor affecting the immune system was the duration rather than the severity of depression. Consequently, in the case of older caregivers, the combination of depression and advancing age delivered a double blow to their immunity.
Curiously, it appears that instead of endeavouring to soothe the population, governments in the West are inadvertently subjecting older individuals, who are already grappling with various stressful issues, to heightened stress levels. This is exemplified by inadequate pensions that fail to cover the cost of living and insufficient access to medical assistance, among other challenges.
Ageing is associated with a natural decline in immune functioning. Immunosenescence is observed in many facets of both innate and adaptive immunity. For example, older individuals have a poorer natural killer cell (NK) response to stimulatory cytokines than younger individuals [1]. Ageing is also associated with impaired activation and proliferation of T- and B-lymphocytes [2]. Furthermore, the B-lymphocytes of elderly individuals produce fewer antibodies than those of younger individuals [3]. In addition, increased production of certain inflammatory mediators is observed during ageing [4]. These immunological changes make older individuals more susceptible to various age-related diseases. However, immunosenescence appears to place older individuals at greater risk when combined with accumulating chronic illnesses, repeated infections, or other external factors [5]. Chronic stress may be one of the factors leaving elderly individuals more vulnerable to age-related diseases [6,7]. https://bit.ly/33y4pRg
Coronavirus Mortality Rate: The Impact of Stress on Immunity
In the early 1980s, psychologists Janice Kiecolt-Glaser, PhD, and immunologist Ronald Glaser, PhD, from the Ohio State University College of Medicine, became intrigued by animal studies that drew connections between stress and infection. Between 1982 and 1992, these pioneering researchers conducted a comprehensive study involving medical students. Their findings were astonishing: the students’ immune responses diminished each year during the stress-inducing three-day exam period. They exhibited a reduced number of natural killer cells, which combat tumours and viral infections. Moreover, their production of immunity-boosting gamma interferon nearly ceased, and their infection-fighting T-cells responded weakly to test-tube stimulation.
These groundbreaking discoveries sparked a surge in research on this topic. By 2004, Suzanne Segerstrom, PhD, from the University of Kentucky, and Gregory Miller, Phd.., from the University of British Columbia, had analyzed nearly 300 studies related to stress and health. Their meta-analysis uncovered intriguing patterns. When people were subjected to stress for a brief period, there was a surge in one type of “first responder” activity, but this was mixed with other signs of weakening. However, when stress persisted for an extended period, whether for a few days or several months to years, as commonly occurs in real life, all aspects of immunity declined. Consequently, long-term or chronic stress due to excessive wear and tear can have devastating consequences on the immune system.
Stress’s Intensified Impact on Vulnerable Elderly Individuals
Suppose stress can suppress the immune systems of healthy individuals. In that case, the repercussions on the elderly, who tend to experience higher levels of anxiety and often have underlying conditions (especially if they adhere to a modern-day diet), are likely to be even more pronounced. In the unfortunate event that they encounter a more potent virus or bacteria, the consequences could potentially be deadly.
The meta-analysis also unveiled that older individuals or those already dealing with illness are more susceptible to stress-related immune alterations. For instance, a 2002 study led by Lyanne McGuire, PhD, from John Hopkins School of Medicine, in collaboration with Kiecolt-Glaser and Glaser, shed light on this issue. The study focused on participants in their early 70s who were caregivers for individuals with Alzheimer’s disease. Those with chronic mild depression exhibited weakened lymphocyte-T cell responses to two mitogens, stimulating the body’s reactions to viruses and bacteria. Remarkably, this compromised immune response persisted even 18 months later, and immunity continued to decline with age. In line with the 2004 meta-analysis, it became evident that the crucial immune factor was the duration, rather than the severity, of depression. Consequently, for older caregivers, the combination of depression and advancing age presented a dual challenge to their immunity.
Stressors and Vulnerable Populations
And voila, that seems to be the case, so instead of trying to calm the population, the governments in the West are doing their best to stress out the older individuals who are already facing other stressful issues. For example, pensions that don’t cover the cost of living or inadequate medical help, etc.
The researchers noted that lack of social support has been reported in the research as a risk factor for depression, an insight amplified in a 2005 study of college students. Health psychologists Sarah Pressman, PhD, Sheldon Cohen, PhD, and fellow researchers at Carnegie Mellon University’s Laboratory for the Study of Stress, Immunity and Disease found that social isolation and feelings of loneliness each independently weakened first-year students’ immunity. https://bit.ly/2Wzv2Ui
To top it, all experts have come up with the term social distancing, which is confusing to many, so they have decided to come up with another term called Physical distancing.
According to Dr Maria Van Kerkhove of the World Health Organization, speaking at a virtual press conference on Friday, the move to use “physical distancing” comes from a desire to highlight “keeping the physical distance from people so that we can prevent the virus from transferring to one another.” https://bit.ly/3bdBzIg
Why invent all these phrases? Why not just say, hey, you know, for a bit of time, it would be better if you don’t get too close to your older relatives as they are the most vulnerable, and this is just a temporary measure. This new term adds more stress to an already stressed out-group (the elderly). The most susceptible become even more vulnerable as their immune systems are further weakened, as stress has been shown to reduce immunity.
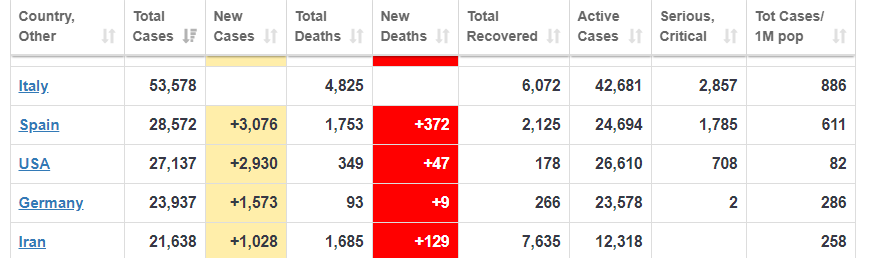
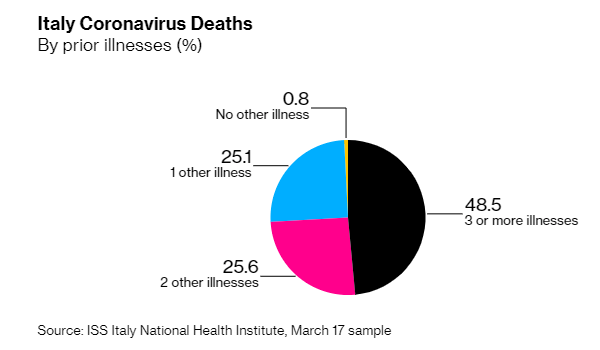
The coronavirus mortality rate in Italy
“The age of our patients in hospitals is substantially older – the median is 67, while in China it was 46,” Prof Ricciardi says. “So essentially, the age distribution of our patients is squeezed to an older age, which substantially increases the lethality.” A study in JAMA this week found that almost 40 per cent of infections and 87 per cent of deaths in the country have been in patients over 70 years old. And according to modelling, the majority of this age group are likely to need critical hospital care – including 80 per cent of 80-somethings – putting immense pressure on the health system. https://bit.ly/3aacIoG
How the deaths are recorded in Italy leaves a lot to be desired. Anyone entering the hospital with a coronavirus diagnosis is deemed to have died due to the coronavirus. Preexisting conditions are not taken into consideration. Remember, an already weakened immune system now has to deal with two or three issues, so assuming the death was due to the coronavirus is nothing short of voodoo science.
Factors Influencing Italy’s High Coronavirus Fatality Rate
“On re-evaluation by the National Institute of Health, only 12 per cent of death certificates have shown a direct causality from coronavirus, while 88 per cent of patients who have died have at least one pre-morbidity – many had two or three,” he says. But other factors may have contributed to Italy’s fatality rates, experts say. This includes a high rate of smoking and pollution – most deaths have been in the northern Lombardy region, which is notorious for poor air quality.
“Doctors in Italy haven’t been dealing with one or two patients in care… but up to 1,200,” says Dr Mike Ryan, health emergencies programme executive director at the World Health Organization. “The fact they’re saving so many is a small miracle.” https://bit.ly/3aacIoG
The data above clearly highlights why Italy has such an abnormally high death rate. This article (clearly) confirms that all studies have already confirmed that those with already compromised immune systems are the most at risk.
More than 99% of Italy’s coronavirus fatalities were people who suffered from previous medical conditions, according to a study by the country’s national health authority. https://bit.ly/3bjhUHg
After deaths from the virus reached more than 2,500, with a 150% increase in the past week, health authorities have been combing through data to provide clues to help combat the spread of the disease. https://bloom.bg/2J6TG6I
Media Fear-Mongering Amid Italy’s High COVID-19 Fatality Rate
Once again, we witness how the media goes to great lengths to induce fear and alarm in the public, painting a grim picture of impending catastrophe. What’s crucial to note is that 99% of those who have tragically lost their lives were already battling pre-existing medical conditions.
Additionally, a significant portion of these fatalities is concentrated in one of Italy’s most heavily polluted regions. When we consider those without pre-existing disorders or conditions, the death rate plummets to a mere 0.8%. Why does the press not emphasize this critical perspective? Why do they persist in alarming the elderly, who are the most vulnerable members of our society? Is there something they’re concealing, or are the healthcare professionals simply overwhelmed with their existing workload? Only time will reveal the answers.
Other Articles of Interest